Introduction: Understanding the Foe
Onychomycosis (pronounced on-ee-koh-my-KOH-sis), derived from the Greek words “onyx” (nail) and “mykes” (fungus), is a persistent and common fungal infection affecting the fingernails or, more frequently, the toenails. It represents a significant portion of all nail disorders, estimated to affect approximately 10% of the global population, with prevalence rising with age – potentially impacting over 50% of individuals aged 70 and above. While often perceived as merely a cosmetic concern, untreated onychomycosis can lead to significant discomfort, pain, functional impairment, and psychosocial distress, impacting quality of life. It also poses a serious risk for secondary bacterial infections, especially in individuals with compromised immune systems or diabetes, where it can be a gateway to cellulitis or more severe complications.
The primary culprits behind onychomycosis are dermatophytes, particularly Trichophyton rubrum and Trichophyton mentagrophytes. These fungi thrive on keratin, the tough protein that makes up nails, hair, and the outer layer of skin. Less commonly, yeasts (like Candida albicans) and non-dermatophyte molds (like Scopulariopsis, Fusarium, Aspergillus) can also invade the nail unit. The infection typically begins at the distal (free) edge or lateral sides of the nail, often entering through small traumas or separations between the nail plate and nail bed (hyponychium). It then spreads proximally, causing characteristic changes.

Table of Contents
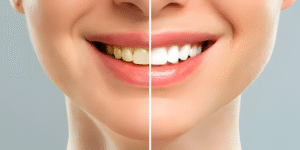
Recognizing the Signs: Symptoms and Clinical Presentations
Onychomycosis manifests in several distinct patterns, though overlap can occur:
- Distal and Lateral Subungual Onychomycosis (DLSO): The most common form. Infection starts under the nail at the tip or sides. Signs include:
- Subungual hyperkeratosis: Buildup of chalky, yellow-white debris under the nail plate, lifting it from the nail bed.
- Onycholysis: Separation of the nail plate from the underlying nail bed.
- Discoloration: Nails turn yellow, brown, white, or even green/black.
- Thickening: Nail plate becomes abnormally thick and brittle.
- Distortion: Loss of the smooth surface, becoming rough or crumbly.
- Superficial White Onychomycosis (SWO): Primarily affects the surface of the toenail plate. Appears as well-defined, opaque, white “islands” or powdery patches on the nail surface that can be easily scraped off. Often caused by T. mentagrophytes or molds.
- Proximal Subungual Onychomycosis (PSO): Less common, starts at the proximal nail fold (cuticle area) and spreads distally under the nail. Often appears as a white or yellow spot near the cuticle that moves forward as the nail grows. This form is more frequently associated with immunosuppression (e.g., HIV) and can be caused by dermatophytes or Candida.
- Endonyx Onychomycosis: Infection penetrates directly into the nail plate without initially involving the nail bed or underside. Causes milky white discoloration within the nail plate, pitting, and lamellar splitting, but usually without significant subungual debris or onycholysis.
- Total Dystrophic Onychomycosis (TDO): Represents the most advanced stage, where the entire nail unit is destroyed. The nail plate is thickened, crumbled, discolored, and often partially or completely detached. This can result from progression of any of the above types.

Prevention: Building a Fungal Defense Strategy
TOP BENEFITS WITHOUT COMPROMISES WHEN IT COMES TO YOUR NAILS & FEET HEALTH 》》》Click now《《《
Preventing onychomycosis is significantly easier than treating it. Key strategies focus on minimizing exposure to fungi and creating an environment where they cannot thrive:
- Meticulous Foot and Hand Hygiene:
- Wash and Dry Thoroughly: Wash feet daily with soap and water, paying special attention to the spaces between toes. Dry completely – moisture is the enemy. Use a separate towel for feet if possible.
- Absorbent Socks: Wear socks made of natural, breathable fibers like cotton or moisture-wicking synthetics. Change socks daily, or more often if feet sweat excessively.
- Alternate Shoes: Avoid wearing the same pair of shoes two days in a row. This allows them to dry out completely inside.
- Protective Footwear in Public Areas:
- Wear Shoes or Sandals: Always wear protective footwear in communal damp areas like public showers, locker rooms, swimming pools, and saunas. Fungi thrive in these warm, moist environments.
- Avoid Barefoot Contact: Refrain from walking barefoot in public places.
- Proper Nail Care:
- Trim Correctly: Keep nails trimmed straight across and filed smooth. Avoid cutting too short or rounding the corners excessively, which can create small injuries for fungi to enter.
- Sanitize Tools: Disinfect nail clippers, files, and other pedicure/manicure tools before and after each use. Avoid sharing these tools.
- Choose Salons Wisely: If getting professional pedicures/manicures, ensure the salon practices strict hygiene protocols, including autoclaving metal instruments and using single-use files/buffers. Bring your own tools if possible.
- Footwear Choices:
- Breathable Shoes: Opt for shoes made of leather, canvas, or mesh that allow air circulation. Avoid tight-fitting, non-breathable shoes (like plastic or vinyl) for prolonged periods.
- Proper Fit: Ensure shoes fit well – not too tight (causing microtrauma) or too loose (causing friction).
- Manage Moisture and Sweat:
- Antifungal Powders/Sprays: Use over-the-counter antifungal sprays or powders inside shoes and on feet daily, especially if prone to sweating.
- Moisture-Wicking Insoles: Consider using insoles designed to draw moisture away.
- Treat Athlete’s Foot Promptly: Tinea pedis (athlete’s foot) is a major risk factor. Treat any fungal skin infection on the feet immediately and thoroughly to prevent spread to the nails.
- General Health:
- Manage Underlying Conditions: Control diabetes meticulously, as high blood sugar impairs immune function and circulation, increasing susceptibility and complication risk. Manage other conditions like peripheral vascular disease or psoriasis affecting nails.
- Boost Immunity: Maintain a healthy lifestyle with balanced nutrition, adequate sleep, and stress management to support your immune system.
TOP BENEFITS WITHOUT COMPROMISES WHEN IT COMES TO YOUR NAILS & FEET HEALTH 》》》Click now《《《
Treatment: Combating the Established Infection
Treating onychomycosis requires patience and persistence, as nails grow slowly and the infection is deeply embedded within a structure that is difficult for medications to penetrate. Success rates vary, and recurrence is common. Treatment choice depends on the type and severity of infection, the causative organism, the number of nails involved, patient comorbidities (especially liver/kidney function), medication interactions, and patient preference.

- Topical Antifungal Agents:
- Best For: Mild to moderate DLSO (affecting <50% of the distal nail plate, without significant matrix involvement), SWO, or as adjunctive therapy to oral medications. Also preferred when oral medications are contraindicated.
- Mechanism: Applied directly to the nail plate and surrounding skin. Newer formulations have better nail penetration.
- Common Agents:
- Ciclopirox (Penlac): Nail lacquer applied daily. Requires weekly removal of accumulated layers with alcohol. Treatment duration typically 48 weeks.
- Efinaconazole (Jublia): Solution applied daily to the nail and surrounding skin. Generally better penetration than ciclopirox. Duration 48 weeks.
- Tavaborole (Kerydin): Solution applied daily. Duration 48 weeks.
- Amorolfine (Loceryl): Nail lacquer applied 1-2 times weekly (available outside the US). Duration 6-12 months.
- Pros: Minimal systemic side effects, low risk of drug interactions.
- Cons: Requires strict, long-term adherence. Penetration is limited, especially for thick nails or deep infections. Success rates (complete cure: clear nail + negative culture) are generally lower than oral therapy (around 15-30% for monotherapy). Requires months of treatment beyond when the nail looks clear.
- Oral Antifungal Agents:
- Best For: Moderate to severe onychomycosis (affecting the nail matrix, >50% of the nail plate, multiple nails), PSO, TDO, or when topical therapy has failed.
- Mechanism: Systemic medication absorbed into the bloodstream reaches the nail matrix (growth center) via the nail bed. As the new nail grows out, it incorporates the antifungal agent, pushing out the infected nail.
- Common Agents:
- Terbinafine (Lamisil): The gold standard for dermatophyte onychomycosis. Typically taken daily for 6 weeks (fingernails) or 12 weeks (toenails). Highly effective against dermatophytes, with cure rates around 70-80%. Fungicidal (kills fungus).
- Itraconazole (Sporanox): Effective against dermatophytes, yeasts (like Candida), and some molds. Often prescribed as “pulse therapy” (one week per month for 2-3 months for fingernails, 3-4 months for toenails). Cure rates similar to terbinafine for dermatophytes. Fungistatic (inhibits growth).
- Fluconazole (Diflucan): Primarily effective against Candida and some dermatophytes. Often prescribed as a weekly dose for 6-9 months (toenails) or 3-6 months (fingernails). Less effective than terbinafine or itraconazole for dermatophytes.
- Pros: Higher cure rates than topicals, treats the infection at its source (matrix).
- Cons: Potential for systemic side effects (headache, GI upset, rash). Requires monitoring of liver function tests (especially terbinafine, itraconazole) due to rare risk of hepatotoxicity. Significant drug interactions possible (especially itraconazole, fluconazole). Not suitable for patients with certain liver, heart, or kidney conditions.
- Laser and Light-Based Therapies:
- Mechanism: Uses specific wavelengths of light (e.g., Nd:YAG laser) to generate heat within the nail plate, theoretically damaging fungal cells.
- Status: FDA-cleared for the “temporary increase of clear nail” in onychomycosis. Considered a treatment option, often when oral/topical therapies are unsuitable or undesired.
- Pros: Non-systemic, no drug interactions, minimal side effects (mild pain, temporary redness).
- Cons: High cost (often not covered by insurance), variable efficacy reported in studies (cure rates generally lower than oral therapy), lack of standardized protocols, often requires multiple sessions. Long-term efficacy data is still evolving. Usually used as monotherapy or adjunctive therapy.
- Surgical/Chemical Nail Removal:
- Mechanism: Physical removal of the infected nail plate (avulsion) either surgically or chemically (using high-concentration urea ointment to dissolve the nail), followed by application of topical antifungal therapy to the exposed nail bed.
- Best For: Severely thickened, painful, or dystrophic nails where medication penetration is impossible, or for a single severely infected nail. Often combined with oral or topical antifungals.
- Pros: Provides immediate relief from pain/debris buildup. Allows direct antifungal access to the nail bed.
- Cons: Painful, risk of infection or damage to the nail matrix (affecting regrowth), the new nail may still become reinfected if antifungal therapy isn’t continued. Not a standalone cure.
- Adjunctive Measures & Important Considerations:
- Debridement: Regular professional removal of thickened, infected nail material by a podiatrist or dermatologist improves topical medication penetration and reduces discomfort. Crucial during treatment.
- Disinfection: Concurrently treat any coexisting tinea pedis (athlete’s foot). Disinfect shoes and socks regularly using antifungal sprays or UV shoe sanitizers.
- Diagnosis is Key: Never self-diagnose or treat. Confirmation via laboratory testing (KOH preparation, fungal culture, or PCR) is essential before starting treatment. Other conditions like psoriasis, lichen planus, trauma, or melanoma can mimic onychomycosis.
- Patience and Adherence: Nails grow slowly (fingernails ~3mm/month, toenails ~1mm/month). It takes 9-12 months for a toenail to fully regrow. Treatment must continue as prescribed, often long after the nail appears clear visually, to eradicate deeply embedded fungus and prevent recurrence. Stopping early is a major cause of treatment failure.
- Managing Expectations: Discuss realistic outcomes and potential side effects with your doctor. Complete cure (100% clear nail + negative lab test) is the goal but not always achieved. Significant improvement is often a more realistic initial target.
TOP BENEFITS WITHOUT COMPROMISES WHEN IT COMES TO YOUR NAILS & FEET HEALTH 》》》Click now《《《
Conclusion: Vigilance and Persistence
Onychomycosis is a prevalent, stubborn, and often frustrating condition. While rarely life-threatening, its impact on comfort, function, and self-esteem can be substantial, and it poses real risks for vulnerable populations. Prevention through diligent hygiene, protective footwear, and managing foot health is paramount. If infection does occur, early diagnosis and appropriate treatment are crucial. A combination of patience, strict adherence to the chosen therapy (whether topical, oral, laser, or combined), regular debridement, and environmental decontamination offers the best chance for success. Consultation with a healthcare professional (dermatologist or podiatrist) is essential for accurate diagnosis, tailored treatment planning, and monitoring throughout the lengthy process of restoring healthy nails. Remember, conquering onychomycosis is a marathon, not a sprint.